People with scars experience pain and discomfort which hinders free movement and the ability to carry out regular activities. Many rely on addictive pain killers for relief. According a report in the ScienceDaily, a study published in the “The Journal of Craniofacial Surgery” suggested that autologous fat grafting could provide the answer to treating scars and resolving the issues associated with the condition when medical and surgical therapies do not work. The researchers reported that “the injection of the patient’s own fat cells is an effective treatment for hard, contracted scars resulting from burns or other causes”.
The researchers used autologous fat grafts to treat about 700 patients with abnormal, painful scars, over a period of six years. All the patients had scarring problems such as hardening or tightening of the skin, which in most cases, limited movement, and could not be improved with other treatments.
The treatment began with liposuction to collect a small amount of the patient’s own fat tissue from the abdomen or hips. After processing – a procedure to remove impurities – the fat cells were injected in the area with the scars. By distributing the fat in various directions and creating a support structure for the scarred, damaged skin, the surgeons found patients gained both functional and aesthetic benefits. Additionally, it was seen that:
- The skin in the scarred area became softer, and more flexible and extensible
- The color of the new skin was similar to the surrounding unharmed skin
- There was decreased pain and increased scar elasticity after the treatment
- Improvements were noticeable in two weeks, progressed through three months, and endured over an year
- Patient reported improved motion in areas where movement was limited due to the tightness and stiffness of contracted scars
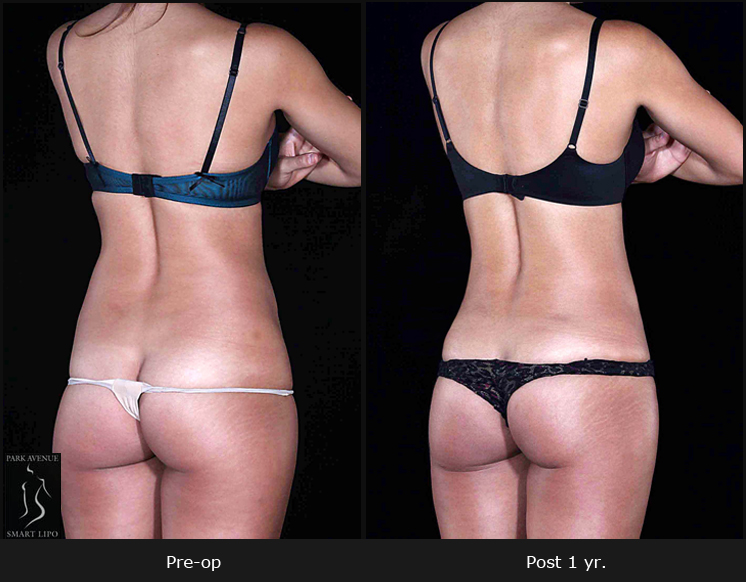
Fat grafting has also won wide acceptance in cosmetic surgery for procedures such as breasts and buttock augmentation, and facial rejuvenation. It is normally an outpatient procedure performed under local anesthesia. The added benefit of contouring the donor site and improved success rates with minimal chances of body rejecting its own tissues contribute to its popularity.