Breast reduction surgery, also called reduction mammaplasty, is a popular procedure that addresses overly large breasts. In addition to aesthetic benefits, the procedure improves a woman’s emotional wellbeing and decreases the physical discomfort and feelings of self-consciousness associated with large, heavy breasts. With advanced techniques, reliable plastic surgery practices provide minimally-invasive liposuction breast reduction using the FDA approved Smartlipo Triplex workstation.
A baseline mammogram may be recommended prior to breast reduction surgery to assess risk of breast cancer. While the American College of Obstetricians and Gynecologists (ACOG) and the American Cancer Society don’t recommend a mammogram until a woman turns 40, a recent University of Michigan study reported that thousands of younger women are receiving a mammogram before reduction mammaplasty. This is a matter of concern as the best guidelines recommend avoiding routine mammograms before elective breast surgery unless a specific concern exists.
In general, breast reduction patients should undergo routine preoperative tests as needed. But a mammogram, which is the only important additional test, should be suggested only for women age 40 and over and those 30 to 40 with a significant personal or family history for breast disease. The researchers found that, each year, many women younger than age 40 with no known breast cancer risk get mammograms. The study did not include women had a personal or family history of breast cancer, genetic predisposition or prior breast disease.
The key findings of the study are as follows:
- 30 percent of women ages 30 to 39 had mammograms before breast reduction surgery, a rate five times higher than that of other women their age
- About 4 percent of women ages 29 and younger received mammograms as they considered breast reduction — compared with 0.2 percent of the population of millennial women.
The researchers noted that the young women in this study probably wouldn’t have had the screenings if they were not having breast reduction surgery, as none of them had a reported breast cancer risk.
Avoiding trivial screenings is actually helpful in terms of time and cost. Beyond that, there are certain risk and limitations for mammograms, which include (Mayoclinic.com):
- It exposes you to low-dose radiation: Though, the dose is very low, for most women the benefits of regular mammograms overshadow the risks posed by this amount of radiation.
- Not always accurate: The accuracy of the procedure depends on the skill of the radiologist and the technique used. Age and breast density is also important factors which might result in false-negative or false-positive mammograms
- Difficult to find in younger women: Breasts of younger women contain more glands and ligaments, resulting in dense breast tissues that can vague signs of cancer. But women over 40 have lighter breasts with fattier breast tissue and have fewer glands, making it easier to interpret and detect changes on mammograms.
- Lead to unnecessary follow-up tests and treatments: Though most abnormal findings detected on mammograms aren’t cancer, the radiologist will want to compare it with previous mammograms or will ask for further testing to confirm this abnormality. Up to 10% of mammograms require additional testing, including additional imaging tests such as ultrasound, and biopsy, a procedure to remove a sample of breast tissue for laboratory testing.
- It can’t detect all cancers: According to Mayo Clinic, mammograms can miss 1 in 5 cancers in women. Some cancers detected by physical examination may not be seen on the mammogram, as it may be too small or may be in an area that is difficult to view such as the armpit.
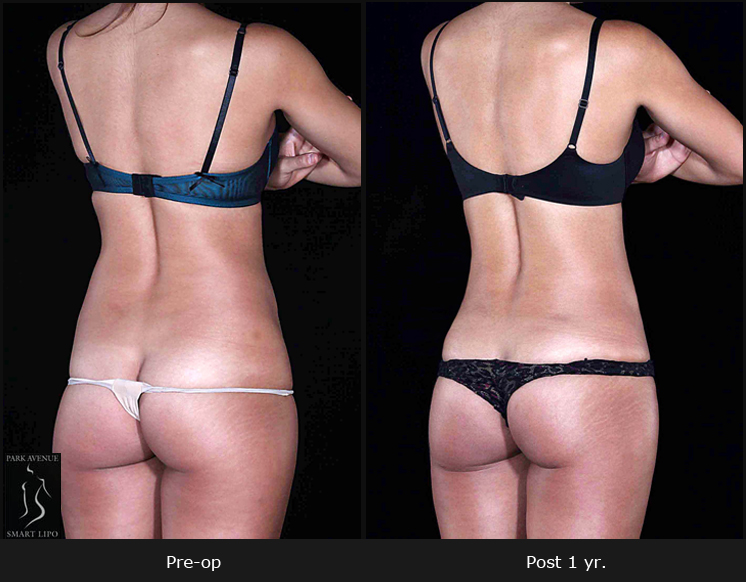
Breast reduction surgery has been consistently reported as one of the highest patient satisfaction procedures because it addresses both functional and aesthetic concerns and positively impacts a woman’s quality of life. Liposuction breast reduction using minimally-invasive Smartlipo laser liposuction device combines three unique wavelengths – 1064 nm, 1320 nm, and 1440 nm – that can be used individually or blended for safe and effective removal of excess fat and skin tightening.
The author concludes that “altering screening mammography for patients younger than 40 years in the setting of evaluation for breast surgery has a risk for subsequent tests and invasive procedures.” She suggests that creating awareness among patients could help reduce these unnecessary screenings. Patients should be motivated to have a conversation with their doctor as to whether they actually need screening mammography.
The American Society of Plastic Surgeons stated in 2014 that women undergoing elective breast surgery should not have additional screening beyond existing guidelines unless there was a concern based on their medical history or a physical finding. Physicians offering breast reduction surgery should be mindful of these guidelines.